What are Medigap Plans?
September 19, 2023 at 9:00 PM
by Tara Taws Claghorn-Nicastro
Rittenhouse Square Insurance
Rittenhouse Square Insurance

Medigap or Medicare Supplement Plan Basics
- Fill the “gaps” that Original Medicare A&B don’t cover
- Can help pay for copays/coinsurance/deductibles of Medicare A & B
- Sold by private insurance companies
- Medicare Supplement Plans are differentiated by letters ( Plan A - Plan N)
- Plans A - N cover different parts of the Medicare A & B deductibles, coinsurance, and copays
- Plans A - N are priced differently
- Standardized = offer same basic benefits regardless of insurance company
- Must follow all federal & state laws to protect you (i.e. be clearly identified, etc.)
- For example, all Medicare Supplement plan Gs have to cover the same basic benefits regardless of the insurance company selling it - what varies is the PREMIUM (price)

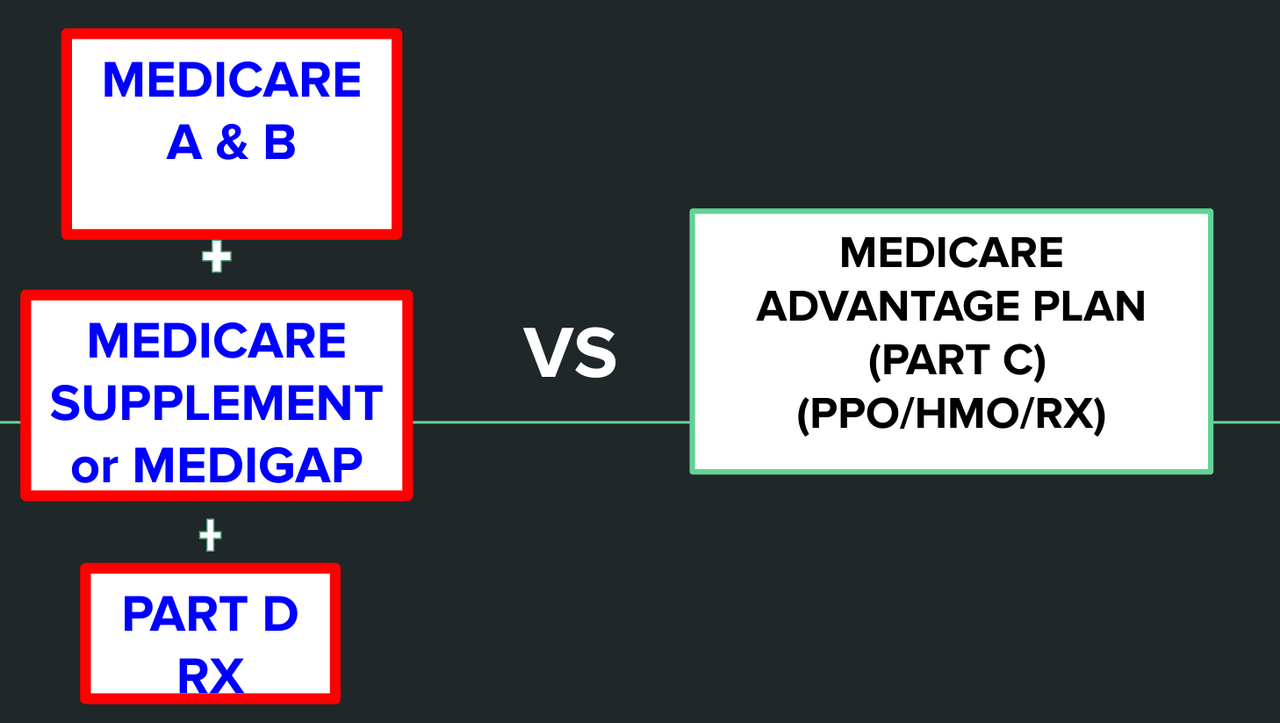
How are Medigap Plans Different from Medicare Advantage Plans?
- Medicare Advantage Plans = another way to manage/get your Original Medicare A & B benefits
- Medicare Advantage PPOs/HMOs manage your Medicare Part A, B and D benefits for you
- The PPO/HMO process your medical claims
- Medigap Plans only help pay for costs that Original Medicare A & B don’t cover
- Medigap plans are secondary insurance to your Original Medicare A & B
- CMS (Medicare) processes your medical claim first, then your Medigap is a secondary insurance and covers some or all of what Medicare A & B don’t cover (depending on Medigap Plan choice/benefit outline)
- Can’t have a Medicare Advantage plan AND a Medigap Plan
- Medigap plans don’t have networks, if provider accepts Medicare, they accept your Medigap
- Medigap plans don’t cover: Vision or Dental Services, Eyeglasses, Hearing Aids
- More and more Medigap plans are coming with Vision, Dental, Eyeglass, and Hearing Aid Discounts
- Medicare Advantage plans often include limited coverage on these services included in their plan
- Note, certain medically necessary vision/dental services are covered by Medicare A, B and Medigap like cataract surgery, diabetic eye exams, glaucoma treatment, etc.
What are the Guaranteed Issue Times to Enroll in a Medigap?
- Guaranteed issue = cover all your pre-existing health conditions and cannot deny or charge you more for a Medigap policy due to past/present health issues
- Initial enrollment period
- Lasts 6 months & begins the first day of the month you’re both 65 or older AND enrolled in Medicare Part B
- Guaranteed Issue period with no medical underwriting
- Medicare Advantage Trial right periods
- Move out of service area
- You are losing employer (retiree/group/union) coverage
- See the 2023 Choosing a Medigap Policy book for other GI enrollment periods
What if I want to enroll in a Medigap at a Non-Guaranteed Issue Period?
- You will be subject to medical underwriting due to past and present medical conditions
- Can be denied coverage
- Can be subjected to higher premiums
To learn more, click the resources and references below or check out my YouTube video about Medigap plans! Stay safe & stay informed!
Resources & References
2023 Choosing a Medigap Policy

Let's talk
We would love to hear from you!